U.S. Army Col. Eric Roberge, MD, radiology consultant for Regional Health Command - Pacific and chief of the department of radiology at Madigan Army Medical Center in Tacoma, Washington, began focusing on mass casualty preparedness while serving as a flight surgeon in Korea in 2001 and then as chief of radiology at the 47th Combat Support Hospital in Anbar Province, Iraq, in 2009. When he returned stateside, Roberge no longer had to respond to combat casualties, but his interest in mass casualty preparedness didn’t wane — in fact, it only deepened as he considered the myriad scenarios in which hospitals across the U. S. might have to respond to mass casualty events, such as natural disasters, transportation and industrial accidents, and terrorism.
Based on lessons learned in combat, Roberge often presented about mass casualty preparedness at professional conferences and frequently studied and talked with colleagues about radiology’s role in responding to potential domestic mass casualty scenarios. But it was two mass shootings — one at a nightclub that left more than 100 dead and injured in Orlando, Florida, in 2016 and another at a concert that left more than 800 dead and injured in Las Vegas in 2017 — that moved Roberge to action.
“It was really after those two big, high-profile incidents that I stopped treating civilian mass casualty preparedness as an esoteric thought experiment and really started to put deliberate action toward developing
my department’s mass casualty plan,” he says. It was an unusual step for a radiologist, many of whom are often left out of mass casualty planning despite radiology’s great potential for improving triage during such events.
Since then, Roberge has become the radiology representative on the trauma committee at Madigan Army Medical Center, a network of healthcare facilities in Washington and California that serves active-duty military members, their families, and veterans. In this role, Roberge has led development of an interdepartmental mass casualty exercise among his hospital’s radiology, emergency, and surgery departments and opened the lines of communication among the departments to develop a robust emergency operations plan that deliberately integrates radiology into the mass casualty response. “We’ve established ourselves as trusted experts who can be relied upon to contribute meaningful work as part of the hospital’s disaster response,” Roberge says. “It’s clear now that we’re a team of teams, not individual teams.”
Recognizing a Need
To start, Roberge reviewed Madigan Army Medical Center’s existing mass casualty preparedness plan, the radiology portion of which dated back to 2002. According to the document, radiology would cancel all of its routine scheduled cases during a mass casualty, and many of the radiology department’s employees would go into the hospital’s labor pool (which often handles moving patients and other ancillary tasks) to support operations in the emergency rooms (ERs) and operating rooms (ORs).

“The problem with radiology going into the labor pool is that radiology is often super busy during a mass casualty,” Roberge says. “If it’s a penetrating mechanism, like a mass shooting, radiology’s role may be more limited, but if it’s a bus crash or a train derailment and everybody has blunt force trauma, all of those people are going to need CT scans. Either way, radiologists are needed to assist with patient care during a mass casualty incident — not just as part of the labor pool.”
As Roberge read the plan, it was clear that the radiology department hadn’t been consulted about its role in mass casualties — something he has found is common at many hospitals. “I have traveled to hospitals around the country, not just military hospitals but civilian ones, and have found that it is a consistent, recurring theme where the radiology portion of the mass casualty plan is written by a non-radiologist,” Roberge explains. “They all tend to say that radiology will supply people to the hospital’s labor pool."
"But pulling radiology employees from their critical work demonstrates a lack of insight into the essential role that radiology plays during a mass casualty," Roberge continues. "If used correctly, radiology can help clinicians more accurately prioritize which patients they should see next and protect critical resources in the hospital, like operating rooms, for those who truly need them. This level of triage can ensure that as many lives as possible are saved.”
Developing an effective mass casualty plan that includes radiology is imperative for all hospitals and health systems nationwide, Roberge says. “It’s important to look at disaster and mass casualty planning not as preparing for something rare or unlikely,” he says. “Disasters don’t just happen in big cities or as part of military operations. There’s a pediatric hospital in Alabama that received about 120 patients following a series of tornadoes. A hospital in Seattle received a busload of international students after a duck boat crash. Hospitals across the country respond to mass shootings almost every day of the week. There are vehicle pileups on icy roads in North Dakota, floods in Houston, and hurricanes and earthquakes in Puerto Rico. Fertilizer factories explode in Wyoming. The point is: This stuff happens everywhere — and it’s our job as physicians to be prepared to respond when it does.”
Engaging Care Partners
Recognizing deficiencies in Madigan’s plan, Roberge began talking informally with clinicians in the hospital’s emergency and surgical departments about radiology’s role in mass casualty events. “I asked them what they needed from radiology during a mass casualty incident and provided various scenarios that could result in mass casualties in the Pacific Northwest,” he says. “For instance, we are in an area known as the Cascadia Subduction Zone, which is a fault line that is overdue for a huge earthquake and tsunami. So I asked them, ‘What would happen if we had an earthquake followed by a tsunami?’”
Roberge received various responses from emergency physicians and surgeons about how they viewed radiology’s role in mass casualty events. For example, one surgeon who Roberge has worked with closely said that he saw radiology as a hurdle to avoid during mass casualties. “He said, ‘I just need to get patients to the operating room really fast, and radiology just slows things down,’” Roberge recalls. “His big complaint was that in a mass casualty, patients are often bleeding to death, and the clock is ticking. He saw radiology as taking a long time, which in his calculus wasn’t worth the investment.”
The feedback challenged Roberge to think about how radiology could improve its response during mass casualty events and other care scenarios. “If I’m not giving the surgeons, one of my internal customers, what they need — rapid, accurate diagnoses — then I’m not doing a good job, and I’m actually becoming a bottleneck to patient flow,” Roberge explains. “I knew I had to come up with ways to provide more efficient service for better triage accuracy.” The conversations also allowed Roberge to demonstrate radiology’s commitment to effective patient care. “If you’re a good, active listener who asks thoughtful questions, people will come to trust your expertise and see that you have good intent,” he says. “You can then build on that relationship to extend influence.”

Most of the emergency physicians and surgeons with whom Roberge spoke were surprised, but not offended, to see a radiologist take the lead in mass casualty preparedness. “Leadership is leadership,” says Lt. Col. Nathan K. Friedline, MD, deputy chief of Madigan’s department of emergency medicine and assistant professor at the Uniformed Services University of the Health Sciences. “I was impressed that Dr. Roberge was stepping out of his normal role to collaborate across departments and improve our response to mass casualty events. These scenarios can be very daunting and scary, so practice and planning among teams beforehand is pivotal. I appreciate his interest in trying to achieve the best-case scenario.”
Identifying Potential Weaknesses
After speaking with ordering providers, Roberge developed a process map to identify weaknesses in
radiology’s workflow, from receiving orders to conveying results to clinicians, during a mass casualty event and other emergency situations. For instance, the hospital planned to switch to electronic health record (EHR) downtime procedures in a mass casualty, meaning it would initially stop using the EHR, allowing response to take priority over documentation of care.
“The problem is that radiology doesn’t run on paper; it runs on computer systems,” Roberge explains. “Under the proposed workflow, you would have to hand-enter paper orders into the radiology information system (RIS), which is time consuming and adds to the concerns that ordering providers expressed about radiology delaying a mass casualty response. So we reflected on the need for radiology to use the EHR for imaging orders in the revised plan.”
Roberge also considered lessons from actual mass casualty events throughout the country. One lesson came from a Boston hospital that received patients from the Boston Marathon bombing, a terrorist attack that killed three people and injured hundreds more in 2013. As is typical, he says, the hospital assigned trauma names to patients until they could identify everyone. Each name was about 30 characters long, but the RIS could display only the first 12-15 characters. “If the stem of every trauma name is identical, you can’t differentiate among patients, which is what reportedly happened during the Boston Marathon bombing,” Roberge says. “They ended up changing their trauma names as a result, and it was something I paid attention to here at Madigan, as we considered shortening our naming conventions.”
In 2017, Roberge was able to further analyze Madigan’s emergency operations plan when the hospital participated in a multistate Federal Emergency Management Association, or FEMA, exercise called Cascadia Rising. The scenario imagined a 10 magnitude earthquake along the Cascadia Subduction Zone, a 620-mile-long fault in Northern California, which triggered a tsunami and destroyed all of the area’s highways and bridges. Roberge concentrated solely on radiology’s response during the exercise, using a 200-pound dummy to determine the throughput rate of trauma patients on one CT scanner. The team found that its throughput rate was reasonable at three to four patients per hour.
Coordinating Care
A few months after Cascadia Rising, Roberge sent an email to about 30 of his colleagues and other care partners about conducting another mass casualty exercise at Madigan in which patients would be transported to different sections for care. “During Cascadia Rising, I was focused on my department, and the ER was focused on operations in the ER, and the OR was focused on operations in the OR,” Roberge says. “I knew everybody was going to do well within their own teams, but the hospital is a team of teams. Patients are handed off as they move from one area of care to another. Transitions of care are where mistakes occur, and I thought it was important to simulate those and identify opportunities for improvement.”
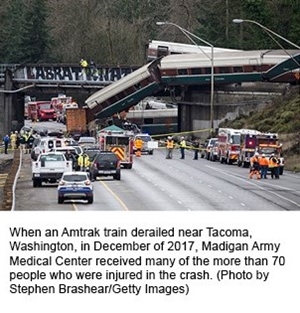
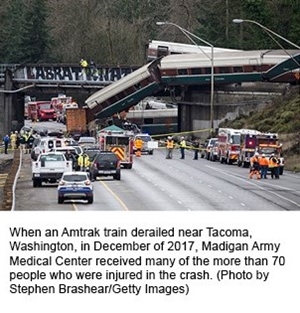
An actual test came just a few days later when Amtrak Train 501 derailed and careened off of a bridge in Tacoma, killing three people and injuring more than 70 others — many of whom were transported to Madigan for care. As patients from the train derailment arrived at the hospital, many of the issues that Roberge warned about came to fruition. “The emergency department was crowded with people trying to be helpful but who were unfamiliar with their roles in the emergency operations plan,” he recalls. “As a result, we had communication issues and challenges identifying and tracking patients.”
Once the emergency was over, Madigan reflected on lessons learned and compiled an after-action report to document what transpired during the event. Hospital leaders recognized that they needed to update their mass casualty plan.
Using an iterative process — from reviewing lessons learned to revising and testing new workflows — they made critical changes and detailed each department’s roles and responsibilities during such an event. For radiology, this involved refining patient naming conventions, honing its communication procedures, tweaking its preliminary reporting methods, and updating its CT protocols for use in mass casualties, says Roberge, who adds that radiology framed this work as a quality improvement project to ensure it was well-resourced and coordinated with the department’s overarching policies and procedures.
With the changes in place, Roberge organized a team to develop a mass casualty exercise to test the revised plan across departments. The core group included two emergency operations center planners, an emergency physician, a trauma surgeon, and a family practice physician. “We also had a broad coalition of hospital staff, including logistics personnel, pastoral services, security services, and clinical services, and we coordinated with our joint partners in the Air Force, as well as state and local partners,” Roberge says. “We expect a real-world response to a mass casualty to include multiple systems of care. As such, we need to be prepared to work seamlessly with our partners.”
Testing the Plan
Over the next eight months, Roberge and the group developed an exercise called Mile Square, which imagined that a C-17 transport plane had crashed into a chapel filled with people on a weekend. “The exercise served as a measurement of progress and after-action review of the fixes that the hospital implemented following the train derailment of 2017,” says David B. Misner, MD, EMS medical director at Joint Base Lewis-McChord and clinical staff attending in the department of emergency medicine at Madigan Army Medical Center, who was involved in planning the exercise. “It was rather unusual to see a radiologist involved, but it was refreshing to see the common goal setting and quantitative approach to a chaotic situation.”
Madigan held the Mile Square exercise a year and a half after the Amtrak train derailment. During the exercise, individual departments — including radiology, emergency medicine, and surgery — got a chance to sharpen their internal operations. But more importantly, the departments tested patient transitions and interdepartmental communications, with radiology central to the response, says Maj. Tyler A. Dailey, MD, radiologist at Madigan. “During mass casualty events, radiology becomes a hub that many clinicians, particularly surgeons, rely on to quickly and accurately identify different injuries and triage patients,” he says.
The exercise showed that many updates to the emergency operations plan improved the overall response. For instance, assigning a specific point of contact within radiology for patients who required immediate surgery ensured more timely care. The exercise also uncovered additional challenges that the team hadn’t considered, including image transfer time for large data sets from the CT scanner to the picture archiving and communication system. When multiple scanners were simultaneously sending 6,000 to 9,000 images across the network, it took as long as 30 minutes for each transfer. This led the team to scrutinize its network performance and to consider scaling down to “bare bones” protocols during mass casualties.
“Many of the things we worked on performed better than they had with the train derailment, though not all,” Roberge says. “It’s one of the reasons why planning and testing should be an iterative and thorough process.”
Preparing to Respond
The Madigan team plans to continue holding similar mass casualty response exercises to ensure everyone remains prepared to respond to an event and to continue to refine its plan as needed. Roberge encourages other hospitals — and radiology departments in particular, given their central role in triaging patients and directing downstream care — to take the time to develop a comprehensive response plan and practice it regularly.
“Radiologists and other physicians must take a close look at their systems to consider how they will function during a mass casualty situation — both the operations within their own departments as well as interfaces with other departments — and how the system can break down,” Roberge says. “It’s something we should be doing every day in preparation for not only mass casualty events but also for efficient and effective daily care delivery — that’s what performance improvement is all about.”
 U.S. Army Col. Eric Roberge, MD, radiology consultant for Regional Health Command - Pacific and chief of the department of radiology at Madigan Army Medical Center in Tacoma, Washington, began focusing on mass casualty preparedness while serving as a flight surgeon in Korea in 2001 and then as chief of radiology at the 47th Combat Support Hospital in Anbar Province, Iraq, in 2009. When he returned stateside, Roberge no longer had to respond to combat casualties, but his interest in mass casualty preparedness didn’t wane — in fact, it only deepened as he considered the myriad scenarios in which hospitals across the U. S. might have to respond to mass casualty events, such as natural disasters, transportation and industrial accidents, and terrorism.
U.S. Army Col. Eric Roberge, MD, radiology consultant for Regional Health Command - Pacific and chief of the department of radiology at Madigan Army Medical Center in Tacoma, Washington, began focusing on mass casualty preparedness while serving as a flight surgeon in Korea in 2001 and then as chief of radiology at the 47th Combat Support Hospital in Anbar Province, Iraq, in 2009. When he returned stateside, Roberge no longer had to respond to combat casualties, but his interest in mass casualty preparedness didn’t wane — in fact, it only deepened as he considered the myriad scenarios in which hospitals across the U. S. might have to respond to mass casualty events, such as natural disasters, transportation and industrial accidents, and terrorism.  “The problem with radiology going into the labor pool is that radiology is often super busy during a mass casualty,” Roberge says. “If it’s a penetrating mechanism, like a mass shooting, radiology’s role may be more limited, but if it’s a bus crash or a train derailment and everybody has blunt force trauma, all of those people are going to need CT scans. Either way, radiologists are needed to assist with patient care during a mass casualty incident — not just as part of the labor pool.”
“The problem with radiology going into the labor pool is that radiology is often super busy during a mass casualty,” Roberge says. “If it’s a penetrating mechanism, like a mass shooting, radiology’s role may be more limited, but if it’s a bus crash or a train derailment and everybody has blunt force trauma, all of those people are going to need CT scans. Either way, radiologists are needed to assist with patient care during a mass casualty incident — not just as part of the labor pool.”
 Most of the emergency physicians and surgeons with whom Roberge spoke were surprised, but not offended, to see a radiologist take the lead in mass casualty preparedness. “Leadership is leadership,” says Lt. Col. Nathan K. Friedline, MD, deputy chief of Madigan’s department of emergency medicine and assistant professor at the Uniformed Services University of the Health Sciences. “I was impressed that Dr. Roberge was stepping out of his normal role to collaborate across departments and improve our response to mass casualty events. These scenarios can be very daunting and scary, so practice and planning among teams beforehand is pivotal. I appreciate his interest in trying to achieve the best-case scenario.”
Most of the emergency physicians and surgeons with whom Roberge spoke were surprised, but not offended, to see a radiologist take the lead in mass casualty preparedness. “Leadership is leadership,” says Lt. Col. Nathan K. Friedline, MD, deputy chief of Madigan’s department of emergency medicine and assistant professor at the Uniformed Services University of the Health Sciences. “I was impressed that Dr. Roberge was stepping out of his normal role to collaborate across departments and improve our response to mass casualty events. These scenarios can be very daunting and scary, so practice and planning among teams beforehand is pivotal. I appreciate his interest in trying to achieve the best-case scenario.”
 Once the emergency was over, Madigan reflected on lessons learned and compiled an after-action report to document what transpired during the event. Hospital leaders recognized that they needed to update their mass casualty plan.
Once the emergency was over, Madigan reflected on lessons learned and compiled an after-action report to document what transpired during the event. Hospital leaders recognized that they needed to update their mass casualty plan. 
