What is an LCD?
An LCD, as defined in §1869(f)(2)(B) of the Social Security Act (SSA), is a determination by a Medicare Administrative Contractor (MAC) regarding whether or not a particular item or service is covered on a contractor–wide basis in accordance with section 1862(a)(1)(A) of the Act. Medicare Administrative Contractors (MACs) establish LCDs.
Local Medicare policies under development in your state
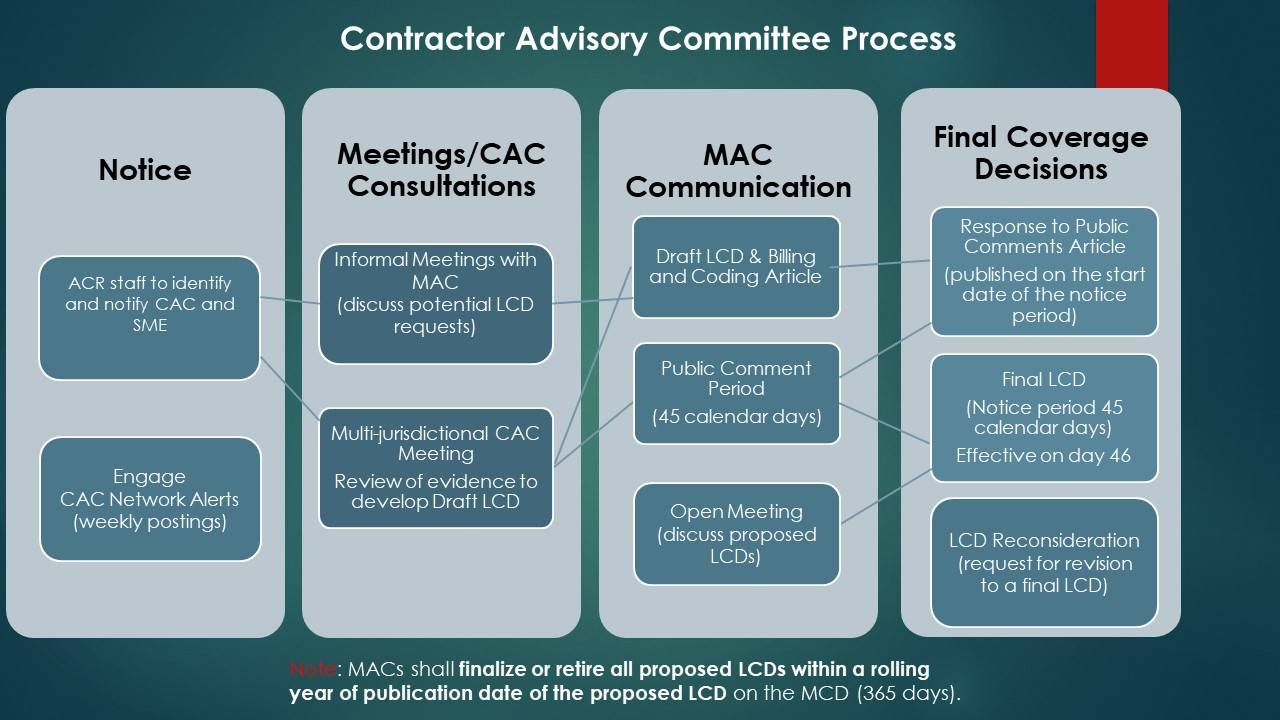
When a Medicare contractor develops a new LCD or significantly revises an existing one, a 45-day public comment period is required. During this time, Contractor Medical Directors (CMDs) solicit input from members of the CAC. Comments can be submitted to the CMD or electronically through your Medicare contractor's website. After the CMDs have considered all comments received, there is a 45-day notice period prior to implementation of the final LCD. Providers and billing staff should track LCD changes using the Medicare Coverage Database. The Centers for Medicare and Medicaid Services (CMS) has revised rules for the development and administration of Medicare Local coverage determinations (LCDs). Learn more about the LCD Modernization Process effective January 1, 2019.
What is the CAC Network?
The ACR CAC Network was developed to encourage communication and coordination among all radiology CAC representatives. The ACR is committed to providing as much assistance as possible to each CAC representative. Adoption of the ACR CAC Networks and the model by the state chapters created a more organized and effective mechanism for dealing with local Medicare issues. State Chapter leaders should notify ACR staff of changes to CAC representatives and alternates.
For questions regarding the CAC Network at the ACR, please contact Alicia Blakey.
CMS Coverage Resources
Principles for Sound Local Coverage Policies
These principles are developed by the ACR and 18 organizations to strengthen the local coverage determination process and engagement of our members with Medicare contractors. The development of sound and effective local coverage policies is driven by a framework that supports successful and consistent communication between Contractor Advisory Committee (CAC) representatives and Contractor Medical Directors (CMDs); inclusion of the most diverse and qualified candidates for input; transparency and adequate opportunities for comment; clear definition of articles and other supporting materials; and Contractor accountability that is measurable and enforceable. These principles allow for Medicare providers to meaningfully participate in the process for developing policy that affects the care they can deliver, and ultimately ensure that Medicare beneficiaries receive the medically necessary care to which they are entitled.