In the 2021 Medicare Physician Fee Schedule (MPFS) Proposed Rule, the Centers for Medicare and Medicaid Services (CMS) chose to move forward with adoption of a new coding structure for the office/outpatient evaluation and management (E/M) codes as recommended by the American Medical Association and the associated increased valuations of these E/M services. In order to maintain budget neutrality with the valuation increases, the proposed CY 2021 conversion factor is $32.2605, a 10.61 percent decrease from the current conversion factor. These changes will result in significant payment reductions to many services, including diagnostic radiology, interventional radiology, nuclear medicine and radiation oncology services in 2021 unless Congress acts to suspend the budget neutrality requirement.
The proposed rule recognizes that there is wide variation in the volume and level of E/M visits billed by different specialties. According to Medicare claims data, E/M visits are furnished by nearly all specialties, but represent a greater share of total allowed charges for physicians and other practitioners who do not routinely furnish procedural interventions or diagnostic tests. Generally, these practitioners include primary care practitioners and certain other specialists such as neurologists, endocrinologists and rheumatologists. These specialties are projected to see reimbursement increases due to the increased relative value units (RVUs) assigned to E/M services despite the decrease in the conversion factor.
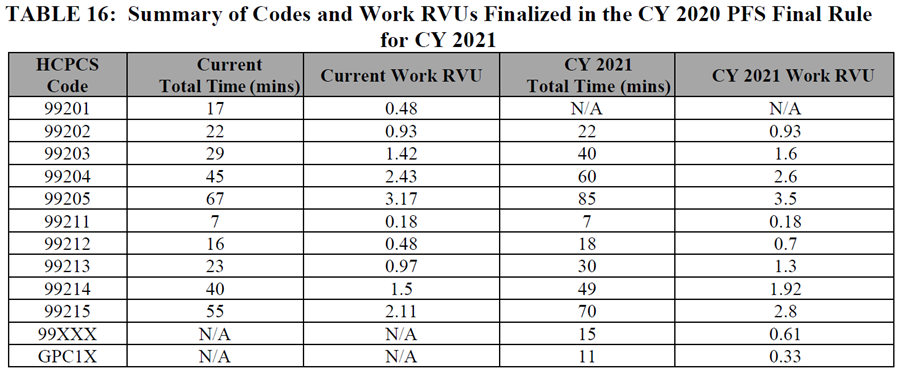
In addition to the new coding structure for E/M visits, CMS also finalized in 2020 rulemaking separate payment for a new prolonged visit add-on CPT code 99XXX and HCPCS code GPC1X, to provide payment for visit complexity inherent to evaluation and management associated with medical care services that serve as the continuing focal point for all needed healthcare services and/or with medical care services that are part of ongoing care related to a patient’s single, serious or complex chronic condition. The addition of these codes also added to the magnitude of the budget neutrality adjustment.
The below table from the proposed rule includes a summary of the codes and work RVUs finalized in the CY 2020 PFS final rule for CY 2021.
CMS reiterated its decision in the CY 2020 MPFS final rule not to make changes to the valuation of 10- and 90- day global surgical packages to reflect changes made to values for the office/outpatient E/M visit codes while they continue to collect and analyze the data on the number and level of office/outpatient E/M visits that are actually being performed as part of these services. In contrast, the agency identified and is proposing to revalue a group of code sets that include or rely upon office/outpatient E/M visit valuation, consistent with the increases in values finalized for E/M visits for 2021. These code sets include end-stage renal disease monthly capitation payment services, transitional care management services, maternity services, cognitive impairment assessment and care planning, initial preventive physical examination and initial and subsequent annual wellness visits, emergency department visits, therapy evaluations, psychiatric diagnostic evaluations, and psychotherapy services. Again, any increases in values in these codes leads to additional budget neutrality decreases.
The American College of Radiology® (ACR®) continues to analyze the MPFS proposed rule and its impacts on radiology services. The ACR is dedicated to mitigating the significant proposed decreases and is working with a large group of stakeholders to develop strategies, including member engagement. Staff will provide additional information on these efforts in the coming weeks. For questions regarding the MPFS proposed rule and impacts on radiology, please contact Kathryn Keysor, senior director, economics and health policy.